1Department of Anesthesia, Providence Healthcare, Department of Anesthesiology, Pharmacology and Therapeutics, University of British Columbia, Vancouver, BC, Canada.
2Department of Anesthesia, Providence Healthcare, Department of Surgery, University of British Columbia, Vancouver, BC, Canada.
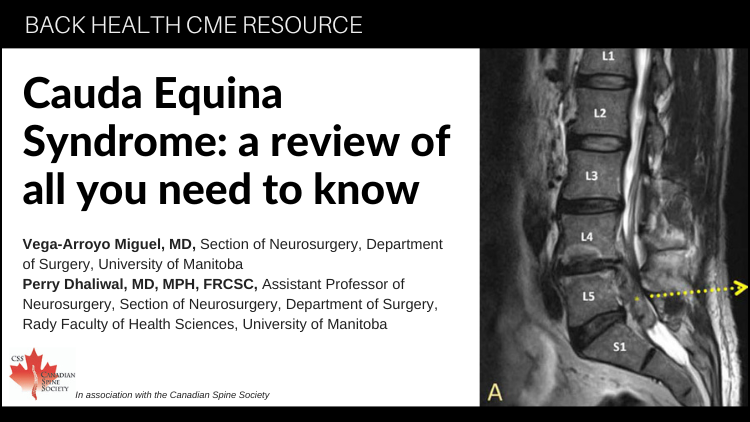
3Department of Surgery, Section of Neurosurgery, University of Manitoba, Health Sciences Centre, Winnipeg, MB, Canada.
4Department of Anesthesia, Providence Healthcare, Department of Anesthesiology, Pharmacology and Therapeutics, University of British Columbia, Department of Surgery, University of British Columbia, Vancouver, BC, Canada.
5Department of Anesthesia, Providence Healthcare, Department of Anesthesiology, Pharmacology and Therapeutics, University of British Columbia, Department of Surgery, University of British Columbia, Vancouver, BC, Canada.