nocturia
Disclaimer:
This article was published as part of THE LATEST IN THE DIAGNOSIS AND MANAGEMENT OF NOCTURIA eCME resource.
The development of THE LATEST IN THE DIAGNOSIS AND MANAGEMENT OF NOCTURIA eCME resource was supported by an educational grant from Ferring Inc.
Nocturia and Nocturnal Polyuria: What Keeps the Urologist Awake at Night
Nocturia and Nocturnal Polyuria: What Keeps the Urologist Awake at Night
Disclaimer:
This article was published as part of THE LATEST IN THE DIAGNOSIS AND MANAGEMENT OF NOCTURIA eCME resource.
The development of THE LATEST IN THE DIAGNOSIS AND MANAGEMENT OF NOCTURIA eCME resource was supported by an educational grant from Ferring Inc.
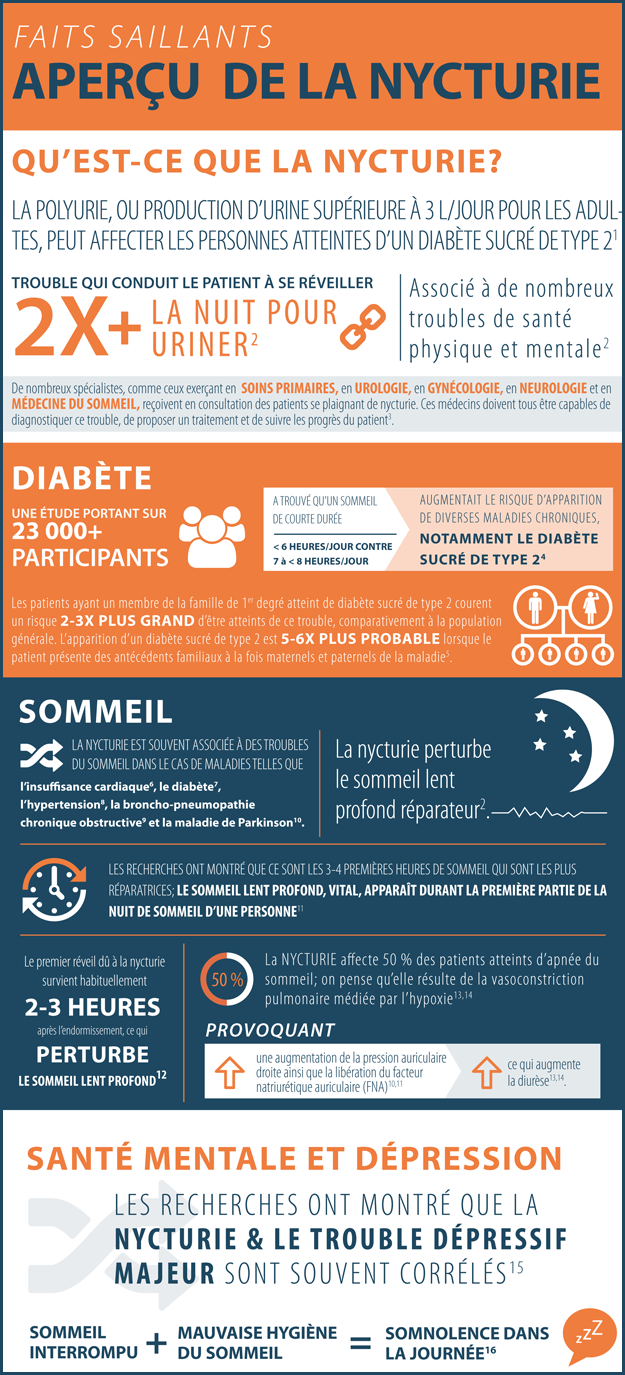
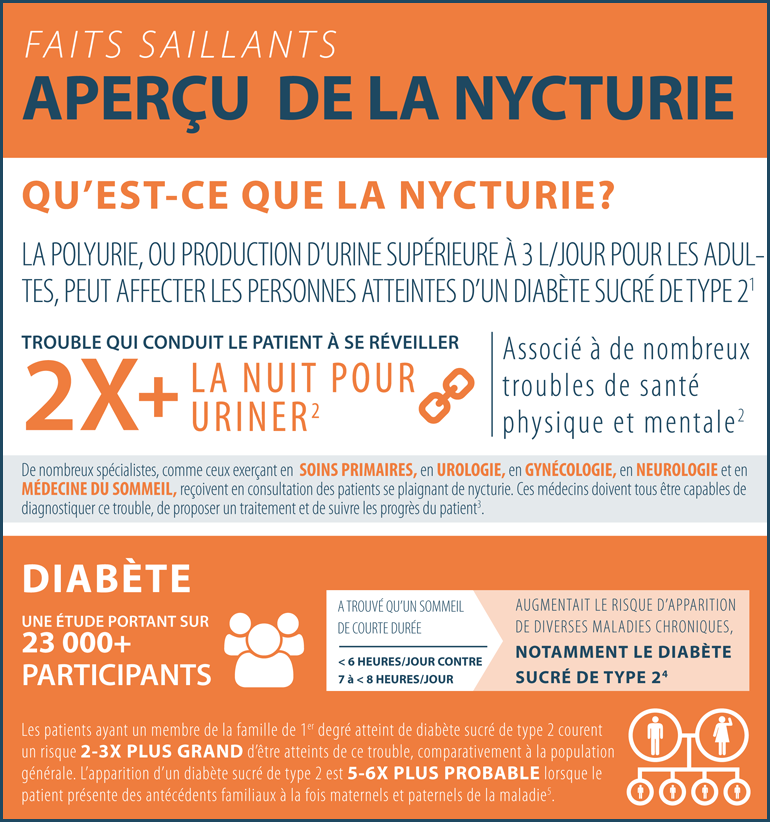
Faits en bref : Aperçu de la nycturie
Faits en bref : Aperçu de la nycturie
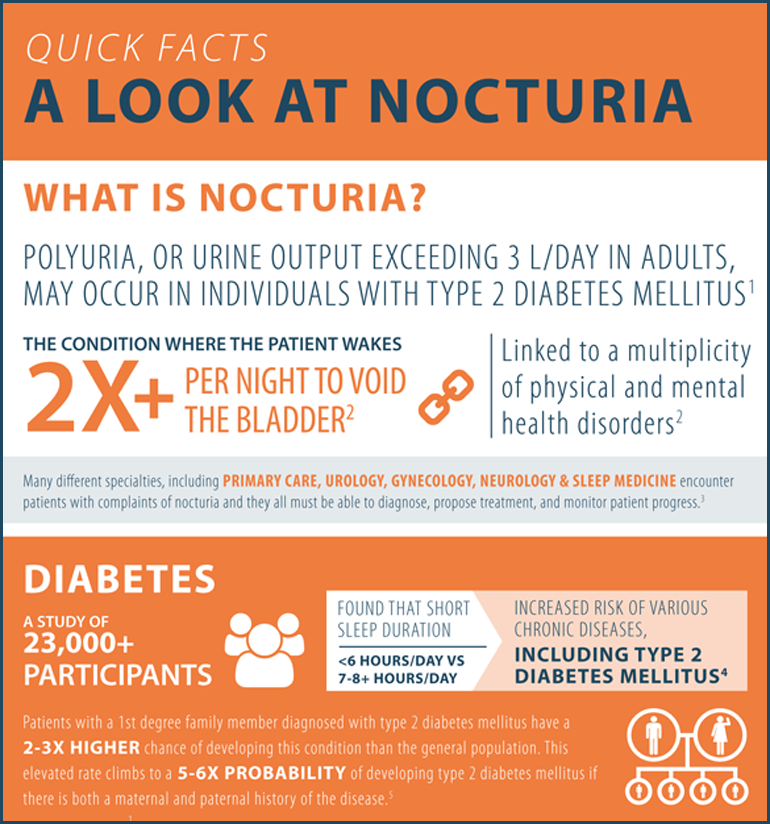
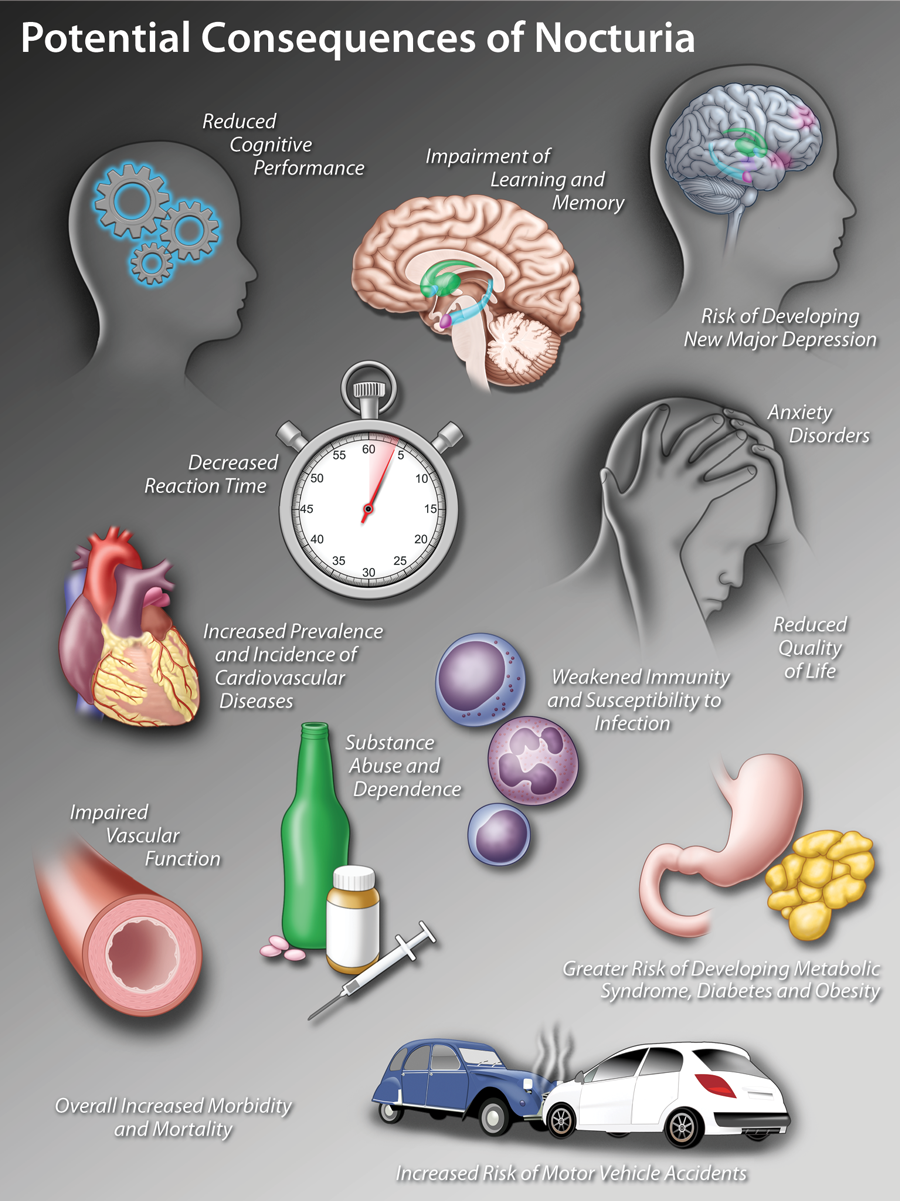
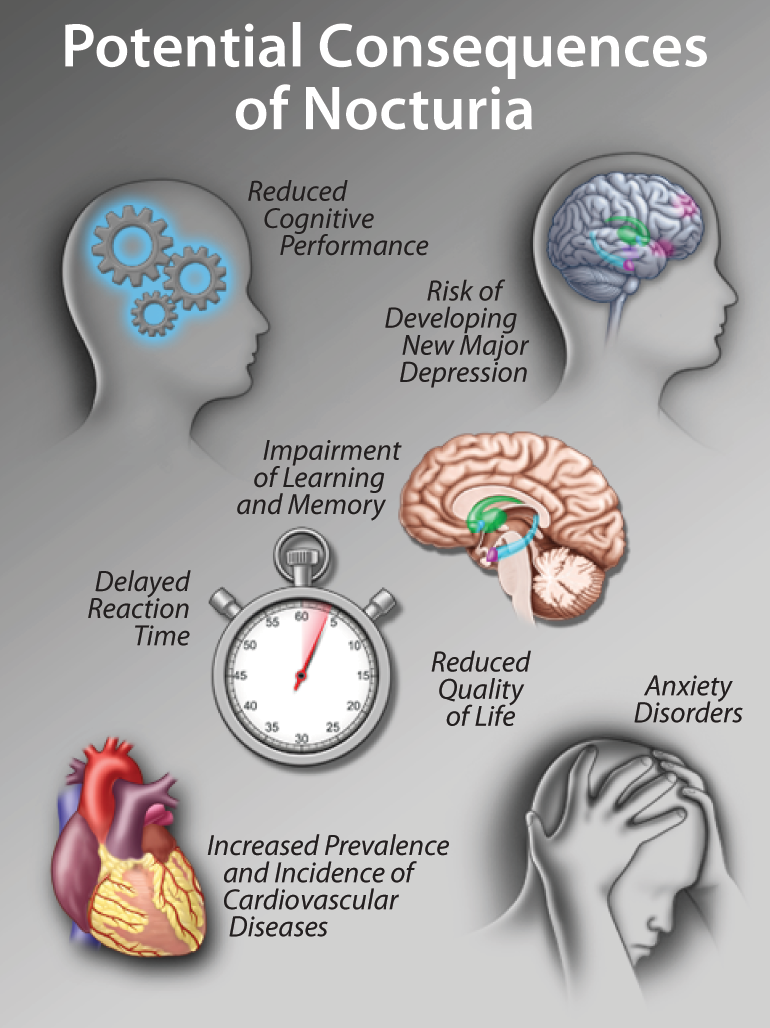
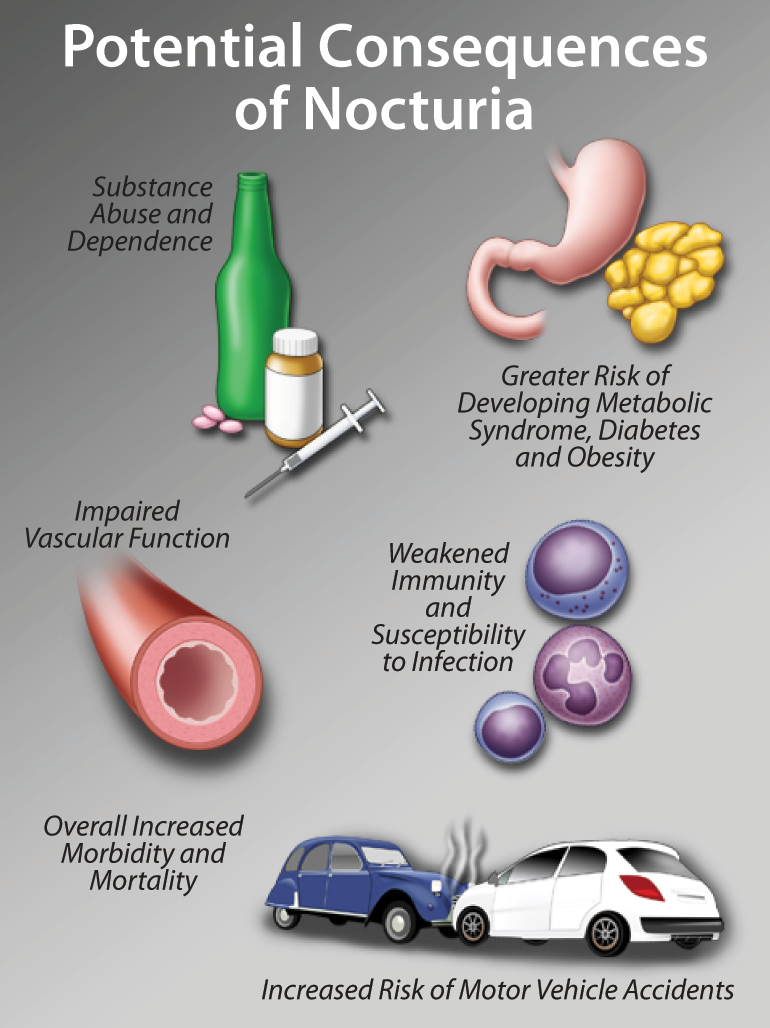
Quick Facts about Nocturia
Quick Facts about Nocturia
Disclaimer:
This article was published as part of THE LATEST IN THE DIAGNOSIS AND MANAGEMENT OF NOCTURIA eCME resource.
The development of THE LATEST IN THE DIAGNOSIS AND MANAGEMENT OF NOCTURIA eCME resource was supported by an educational grant from Ferring Inc.
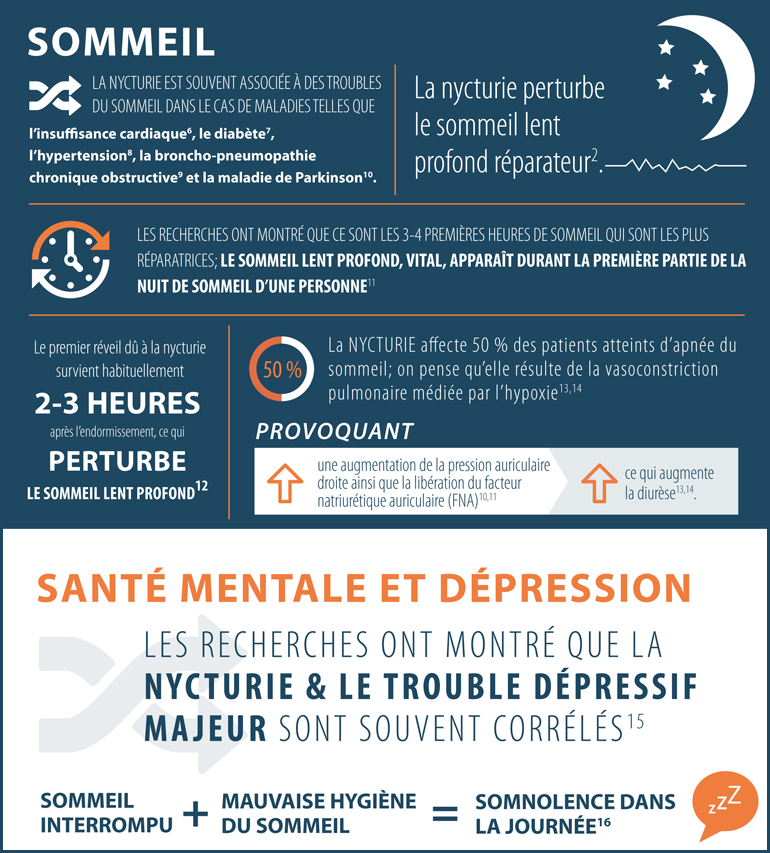
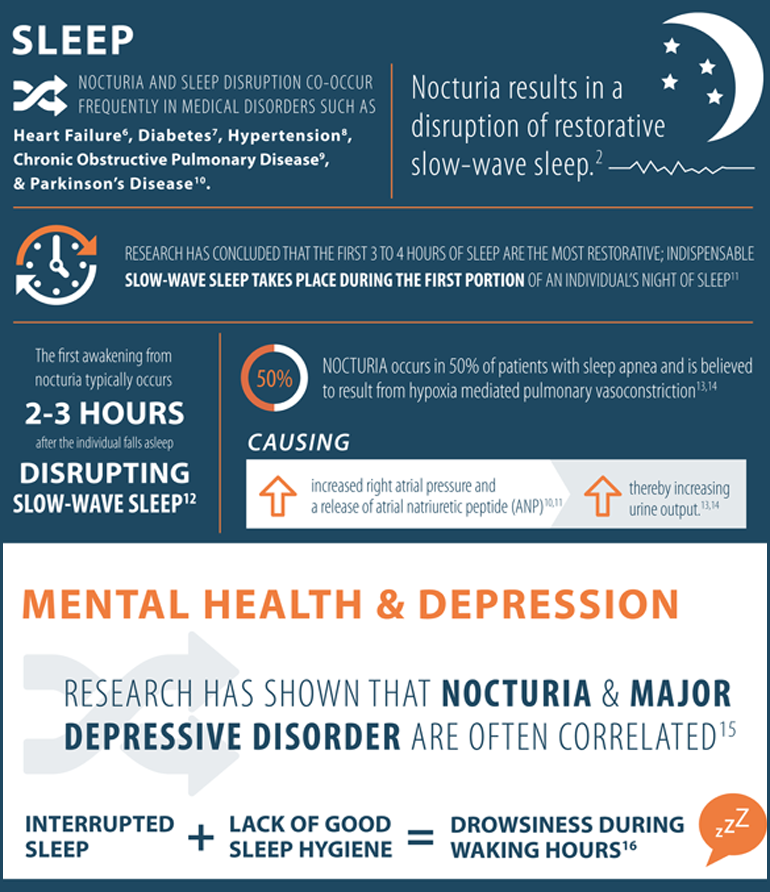
Nocturia and Sleep Disorders
Nocturia and Sleep Disorders
Disclaimer:
This article was published as part of THE LATEST IN THE DIAGNOSIS AND MANAGEMENT OF NOCTURIA eCME resource.
The development of THE LATEST IN THE DIAGNOSIS AND MANAGEMENT OF NOCTURIA eCME resource was supported by an educational grant from Ferring Inc.
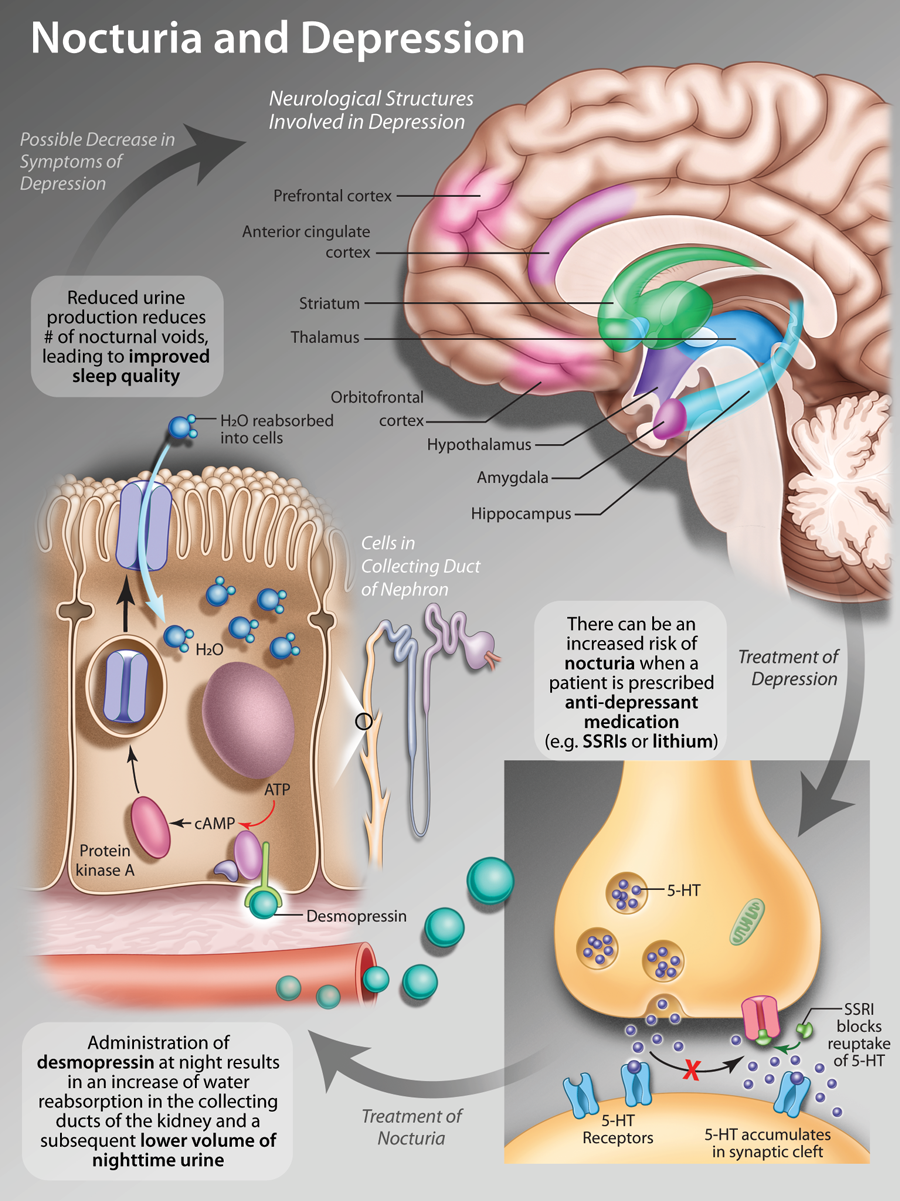
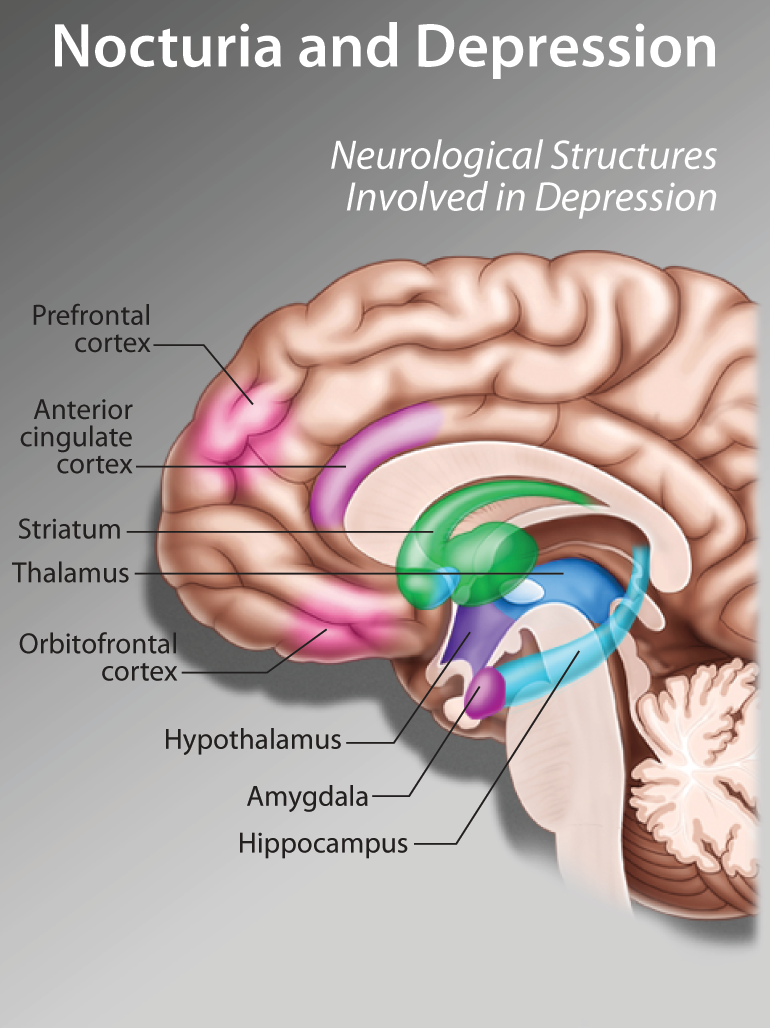
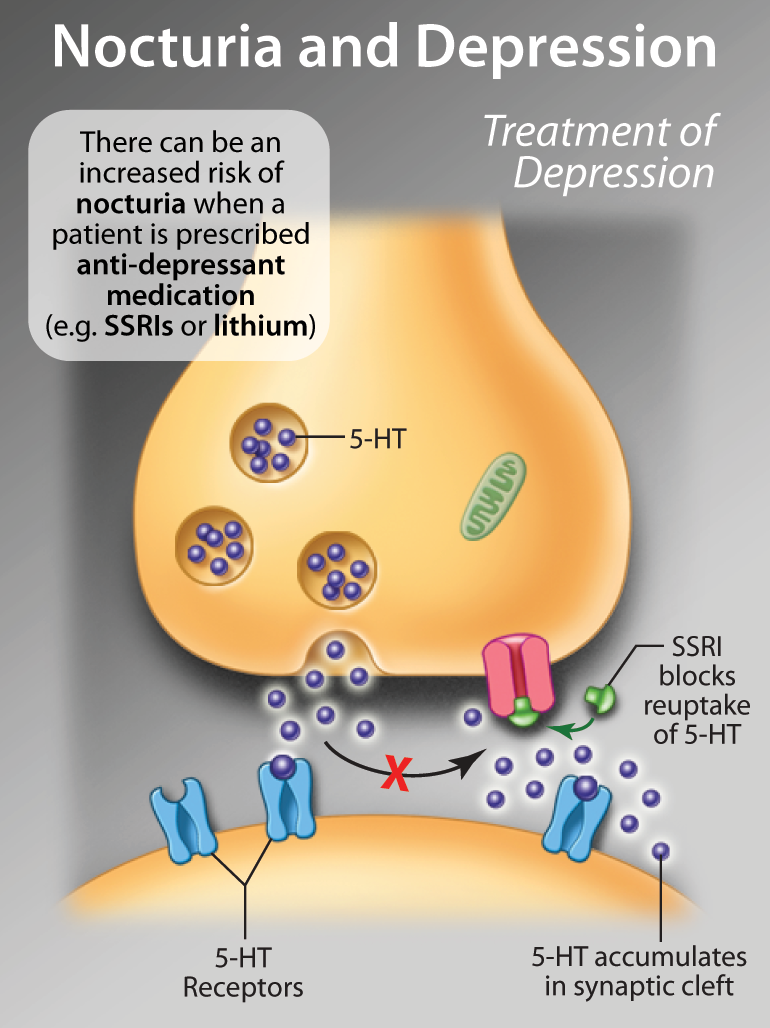
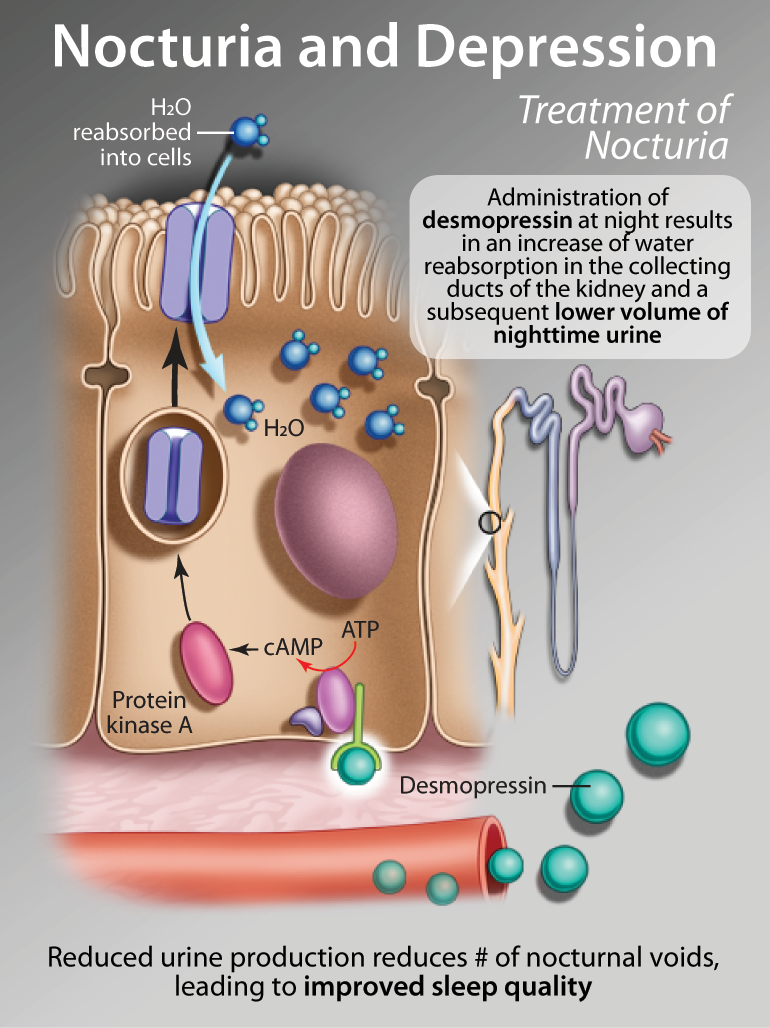
Nocturia and Major Depressive Disorder
Nocturia and Major Depressive Disorder
Disclaimer:
This article was published as part of THE LATEST IN THE DIAGNOSIS AND MANAGEMENT OF NOCTURIA eCME resource.
The development of THE LATEST IN THE DIAGNOSIS AND MANAGEMENT OF NOCTURIA eCME resource was supported by an educational grant from Ferring Inc.