Eric M. Morrow, MD, PhD, Department of Psychiatry, Massachusetts General Hospital, Boston, MA, USA.
William E. Falk, MD, Department of Psychiatry, Massachusetts General Hospital, Boston, MA, USA.
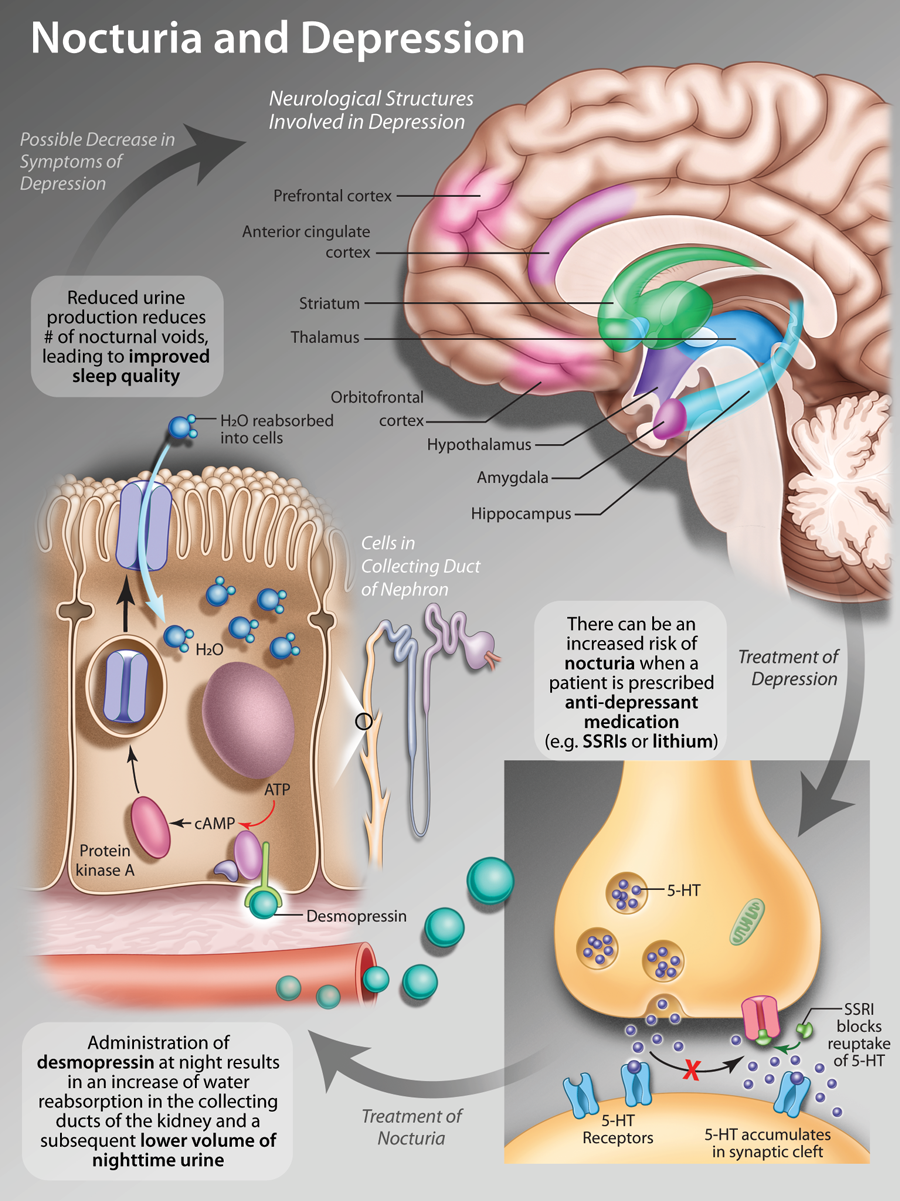
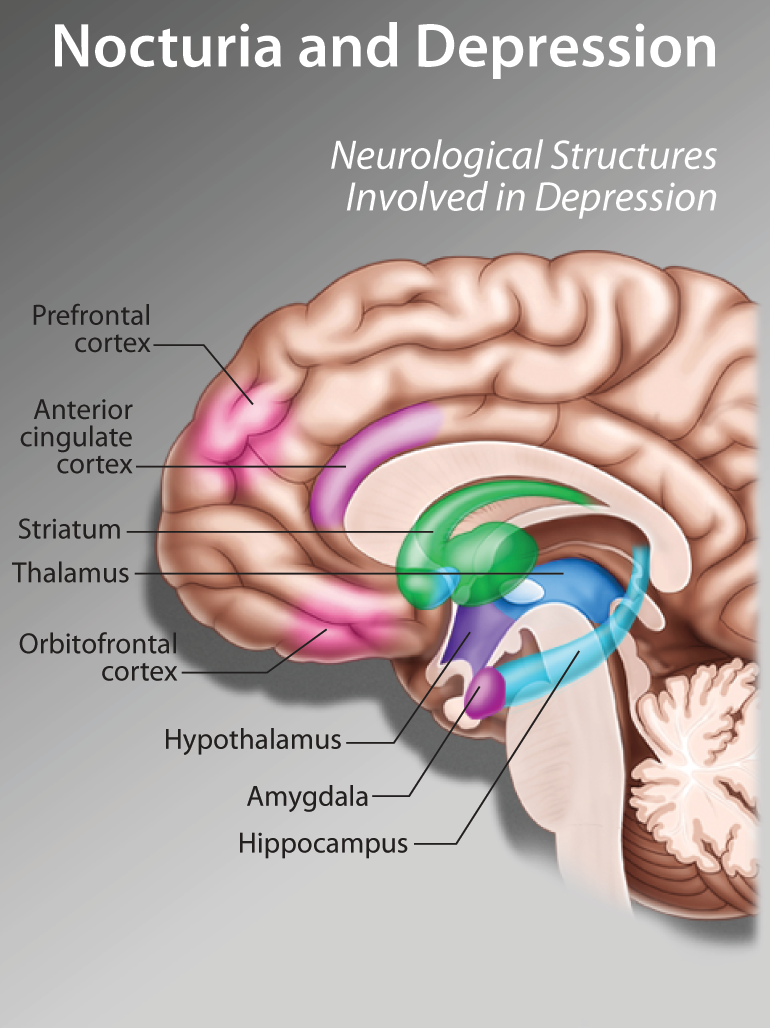
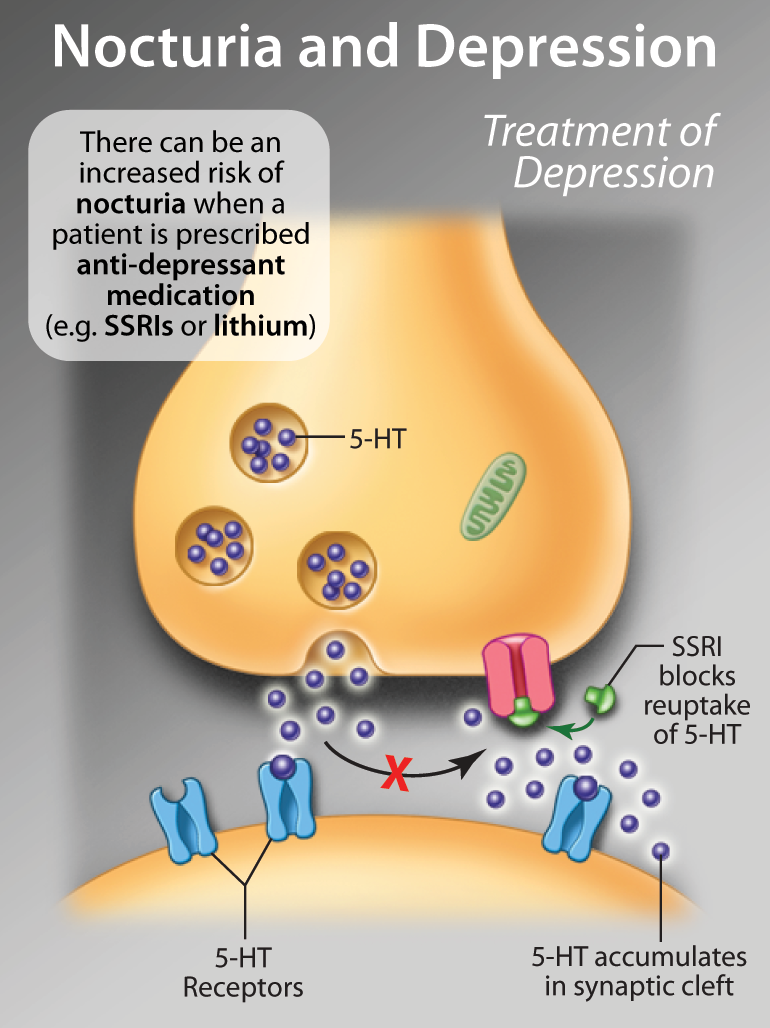
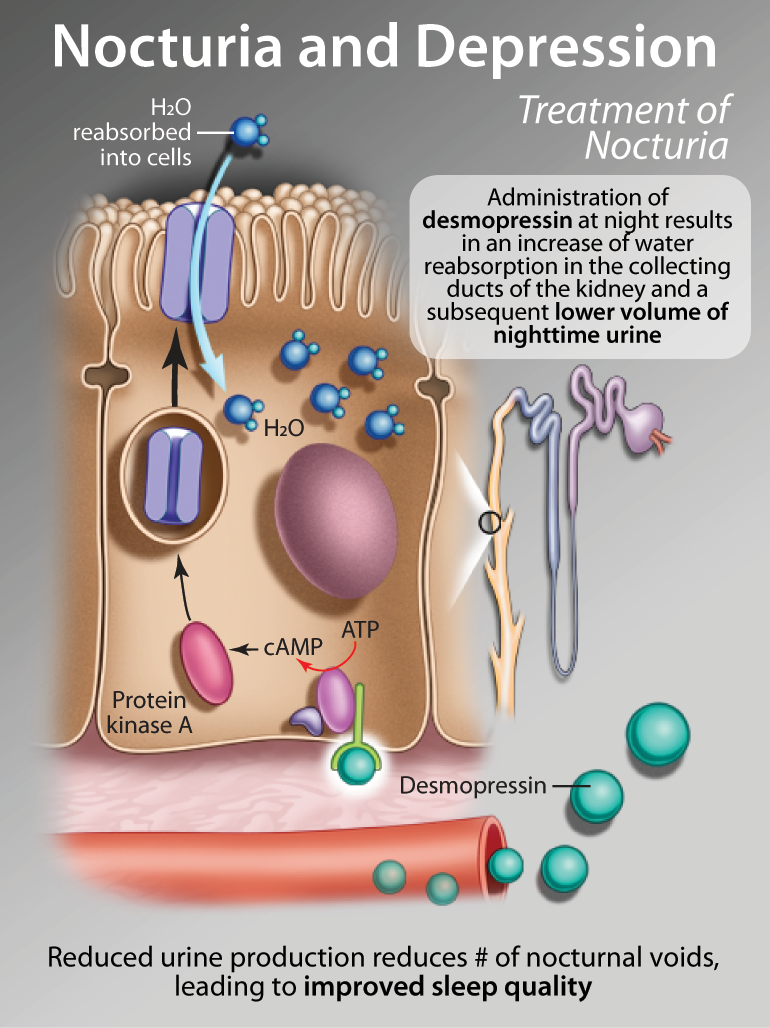
Anxiety in older patients, when excessive in degree and duration, can cause significant impairment and, if left untreated, may result in profound comorbidity--in particular, depression. Anxiety symptoms emerging in the older patient necessitate an extensive medical and psychosocial workup. There is a paucity of data for pharmacological treatment of anxiety disorders in older adults. In this review, we will discuss some of the research in the area of diagnosis and treatment of anxiety in older adults. We will also summarize some practice parameters common in our clinic when data are absent or lacking. The use of psychotherapies (such as cognitive behavioural therapy) and of medications such as the SSRIs, as well as benzodiazepines and other agents including the atypical antipsychotics, are discussed. The differential diagnosis of anxiety symptoms in the older patient, including careful attention to underlying medical and neurologic causes of anxiety, are emphasized.
Key words: SSRIs, benzodiazepines, psychotherapy, anxiety, depression, dementia.