Click here to view the entire report from the 28th Annual Scientific Meeting of the Canadian Geriatrics Society
Frailty: Searching for a Relevant Clinical and Research Paradigm
Speaker: Howard Bergman, MD, The Dr. Joseph Kaufmann Professor and Director Division of Geriatric Medicine, McGill University, Montreal, QC; Co-Director: Solidage Research Group, Montreal, QC; Director, Quebec Research Network in Ageing/Fonds de Recherche en Santé du Québec, Montreal, QC; Chair, Advisory Board, Institute of Aging, Canadian Institutes of Health Research, Ottawa, ON.
The term frailty, observed Dr. Howard Bergman, is widely used by health professionals who treat aging adults. Nonetheless, the concept remains ill-defined. What is it, what are its components, and how is it measured in the clinical setting? Does the term add something to the effort to mitigate adverse health outcomes among older adults?
Conceptualizing Frailty and Understanding the Aging Process
The challenge of studying frailty, Dr. Bergman maintained, is the lack of clear criteria to designate it. How frailty differs from disability, and how researchers and clinicians define effects of aging versus markers of frailty are areas of evolving medical knowledge. The result is that clinicians are utilizing the concept without agreement on its meaning, a problem exacerbated by the fact that frailty is a nonmedical term circulating in popular language.
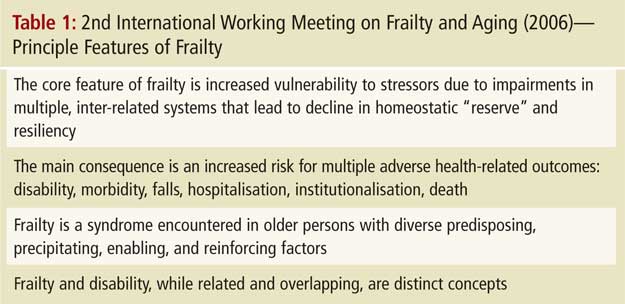
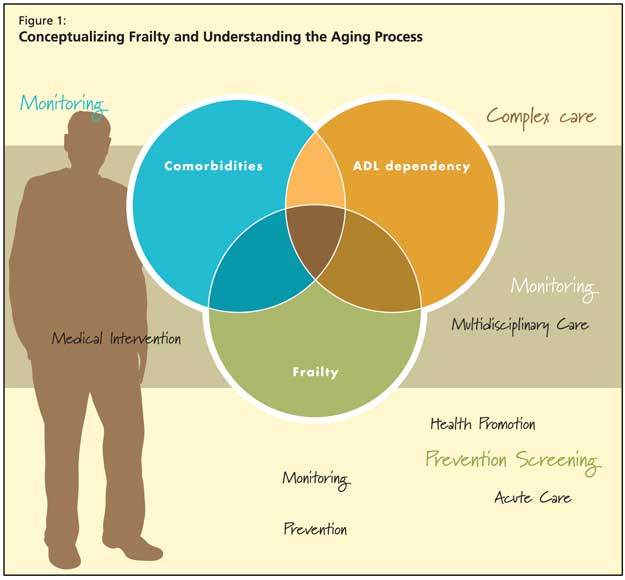
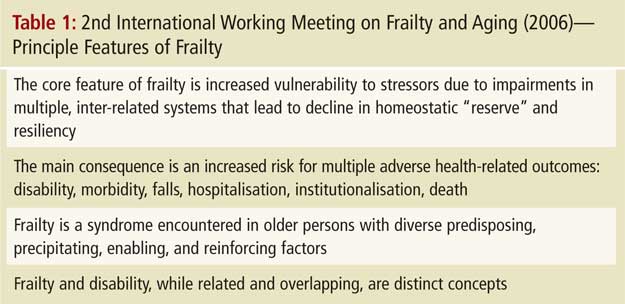
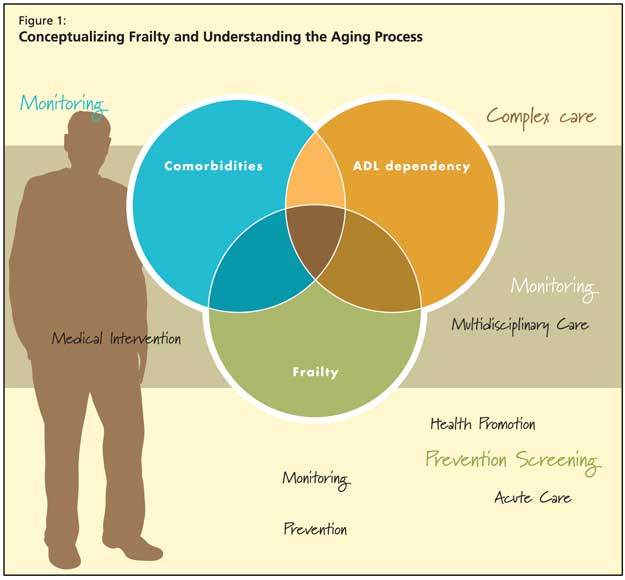
The 2nd International Working Meeting on Frailty and Aging held in Montreal in March of 2006 sought to address key issues and controversies related to the concept of frailty. The core features agreed upon are presented in Table 1. Participants concurred that frailty is “an increased vulnerability to stressors due to impairments in multiple, inter-related physiologic systems.” These impairments are believed to lead to declining homeostatic reserve and resiliency. The working group acknowledged that while frailty and disability have overlap, they remain distinct concepts (Figure 1). A key feature of frailty is that it is associated with increased risk of morbidity and mortality, stated Dr. Bergman.
Frailty has been described with various combinations of components including physiological abnormalities, impairments in physical, cognitive, and/or psychological function, and other features such as advanced age.
According to Dr. Bergman, research strategies that use the life-course approach can significantly contribute to the current understanding of frailty. This individualized, integrative approach conceives that how one ages is a product of factors across the whole life span—including environmental exposures, genetic predispositions, and health behaviours. Critical factors across the life course may determine whether one ages healthfully or not. This research and clinical approach attempts to elucidate the heterogeneity of functional decline in older people.
Ongoing Controversies in Defining and Using the Frailty Concept
Frailty is not yet a clinical instrument. Controversies and grey areas that persist include disentangling chronic disease states from frailty. Dr. Bergman described the two as bearing a complex relationship: there is some overlap, but the key distinction is that while most frail persons have chronic disease, most people with chronic disease are not frail. There is a distinct increase in the prevalence of frailty when the number and severity of chronic diseases increase. Whether frailty is a secondary condition rather than an underlying state is still being explored. Further, being frail and having a high index of comorbidities are not equivalent. It is important to consider contextual issues in health care—for example, studies suggest that patients with poor access to health care will show higher degrees of frailty.
Dr. Bergman highlighted that there is a spectrum of frailty models. At one extreme of the spectrum frailty is represented as a medical syndrome and at the other it is a group of risk factors (Table 2).

In viewing frailty as a syndrome with defining core features, Dr. Bergman suggested that there may be important lessons to be learned from the metabolic syndrome. As with frailty, there is debate and controversy about the clinical definition of the metabolic syndrome. As syndromes, the presence of multiple components are expected have a stronger association with adverse outcomes than the sum of the individual components.
Dr. Bergman acknowledged the disadvantages associated with increasing utilization of the frailty concept. For example, physicians may overvalue the symptom cluster, thereby overlooking the possible value of a single symptom. In addition, some of the measures proposed for frailty such as gait velocity or grip strength do not have established cut-offs, thereby making it difficult to determine how to classify individuals. Further, introducing “frailty” as a diagnosis in clinical practice carries the potential danger of inappropriate labeling, which can have various negative effects on a patient’s health state and health-related decision-making.
However, Dr. Bergman stated, the concept of frailty also holds great potential value for physicians, as it has functional utility in clinical practice. The term identifies a subset of vulnerable older adults at high risk of adverse outcomes. The health needs of older persons who are functionally independent, with apparently normal cognitive function, may be overlooked if clinicians disregard identifiable frailty markers.
Frailty markers provide health care planners with the ability to make valuable predictions, according to Dr. Bergman. A wider clinical application of the concept could improve understanding of the aging process and enhance clinicians’ ability to characterise the heterogeneity in the health of older persons. With an aging population, the capacity to better target and remediate risk in nondisabled older adults with chronic disease could lead to better tailoring of health interventions, and correspondingly, improved health outcomes. For example, Dr. Bergman cited a study that found that patient care measures that delayed the onset of disability and/or dependence by only 1 or 2 years reduced needs for long-term care and institutional resources significantly.
Conclusions and Recommendations
Dr. Bergman concluded that while research and debate on frailty has improved understanding of aging adults, the concept retains at present more potential than practical and acknowledged utility. Ultimately the test of frailty’s relevance will lie in further research initiatives on frailty and whether medical professionals succeed in improving health promotion, prevention, treatment, rehabilitation, and care interventions for aging adults.